Pharmaceutical Sales Data
Pharmaceutical sales data is the collection of sales transactions from drug manufacturers, wholesalers, and mail order pharmacies that make up a product's total sales. All product sales originate in the drug manufacturer. The product may get resold one or more times until it reaches the patient. Therefore, sales data transactions may capture the sale of the same unit of the product more than once.
IMS HEALTH's DDD sales data introduces rules to avoid the double counting of transactions, keeping the one closer to the point-of-care outlets. For example, for wholesalers reporting their sales data to DDD, sales transactions from manufacturer into these wholesalers are omitted. Or, when a wholesaler supplies another, and the second wholesaler reports their sales data to DDD, the transactions between the two wholesalers are omitted.
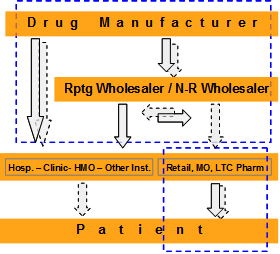
At the same time, DDD sales data accounts for non-reporters by taking a step above to capture the sales into the non-reporter by the supplying entity. Thus accounting for almost every sale made within the distribution system.
Although the great majority of the transactions are conducted between wholesalers and healthcare providers, the manufacturer transactions are as much a part of DDD sales data. DDD sales data uses these transactions to account for any direct sales by the manufacturer to healthcare outlets, and sales to non-reporting wholesalers. The significance of a manufacturer's direct sales depends on the its level of direct sales.
Pharmaceutical sales data in general is subject to a certain level of data blocking that affects the overall completeness of the data. Data blocking is initiated usually by healthcare accounts or payers that want their data withheld from the sales data stream. Despite all that, DDD sales data is the gold standard for measuring total list-price sales for pharmaceutical products.
Applications of pharmaceutical sales data include total product sales performance, market share calculations, manufacturing demand forecasting, sales forecasting, ROI analysis, account targeting, sales force compensation, opportunity assessment, company valuations, licensing, competitive intelligence, contract performance, etc.
'Pharmaceutical Sales Data 101, The Client Perspective', 'Pharmaceutical Sales Data 101, Workbook', and 'Pharmaceutical Sales Data, Just for Sales Reps' provide thorough coverage of DDD sales data.
Prescription Data
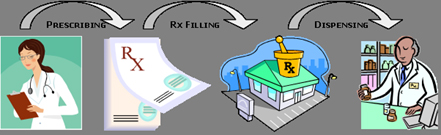
Prescription data is a collection of retail, mail order, and long term care pharmacy transactions. The purpose of prescription data is to capture a physician's prescribing activity for each pharmaceutical product and use the data to direct marketing efforts towards those physicians with either high activity or potential. IMS HEALTH' Xponent data is a premier commercial database capturing prescription data for the US pharmaceutical market.
Prescription data originates at the physician office and the prescription pad. When a prescription slip is presented at a pharmacy, the prescriber and dispensed drug information is captured in the pharmacy's computer system to form the basis of prescription data. The other relevant information such as quantity dispensed, days of therapy, and drug information stored in the pharmacy's own databases, provide the required data elements that go into the Xponent prescription data.
For retail and long-term-pharmacies, Xponent collects large data samples from which it projects the remaining prescriptions. Because mail order does not have predictable patterns from which to project the data, mail order prescription data is un-projected in Xponent. Because Xponent covers only the pharmaceutical retail channel, the data does not represent total product performance.
Applications of prescription data include product performance, market share calculations, forecasting, ROI analysis, prescriber targeting, sales force compensation, opportunity assessment, licensing, manufacturing demand, contract performance, etc.'Pharmaceutical Sales Data 101, The Client Perspective', 'Pharmaceutical Sales Data 101, Workbook', and 'Pharmaceutical Sales Data, Just for Sales Reps' provide thorough coverage of Xponent prescription data.
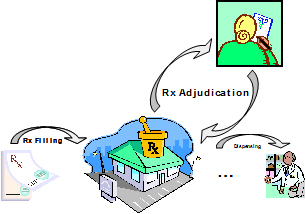
Payer Reimbursement Data
Payer reimbursement data comes from the same transactions that make up the prescription data. It takes advantage of the payer attributes in the transactions between the pharmacy and the Pharmacy Benefit Manager (PBM) adjudicating the prescription. Adjudication is the process PBMs undertake to determine patient enrollment and eligibility with the reimbursing healthcare plan, and determining the financial responsibilities of the payer and the patient for to the present transaction. That includes the patient's co-pay, co-insurance, deductible, and the pharmacy's amount of reimbursement from the payer.
IMS HEALTH's Xponent PlanTrak is one the industry's premier payer reimbursement data products. Xponent PlanTrak captures payer reimbursement only from retail and LTC pharmacies through the same Xponent prescription data, and projects it to the national universe of these pharmacies.
Applications of prescription data include product and payer performance, market share calculations, ROI analysis, payer targeting, sales force compensation, contract performance, etc.
'Pharmaceutical Sales Data 101, The Client Perspective', 'Pharmaceutical Sales Data 101, Workbook', and 'Pharmaceutical Sales Data, Just for Sales Reps' provide thorough coverage of Xponent PlanTrak payer reimbursement data.
Longitudinal Patient Data
Unlike prescription data that is limited to the patient's drug therapy, longitudinal patient data taps into information on the patient's total care. That includes physician visits, hospitalization, long term care therapy and other outpatient care, and drug therapy. The data is to study provider, patient and payer behaviors over time (longitudinally) with respect to care in order to improve medical outcomes, establish cost/benefit benchmarks, and maximize the commercial opportunity of drugs.
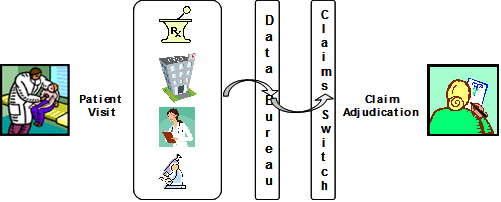
Patient data originates not only in places where care is provided, but with payers, service providers and other aggregators of information like government organizations. All healthcare provider sites have the potential of generating patient data whether that is making a diagnosis, measuring biometric information, administering a lab test, performing a procedure, administering a drug, etc. Payers collect information on their covered patients from healthcare providers, but they also generate financial information that is used to measure the burden of illness. Software vendors providing automation solutions are often data aggregators from the many sites they service. Claims switches that route information between providers and payers are also aggregators of longitudinal patient data.
There are two main types of patient data based on two key processes. The first is related to providing and recording patient care. This takes place within the healthcare sites and is meticulously detailed. Electronic recording of this data requires specialized software systems referred to as Electronic Medical Record (EMR) systems. The caveat with this process is that to-date electronic recording of the data is not very widely used. EMR data is particularly useful in dosing and disease stage studies.
The second is related to the reimbursement of the care provider, and that is where part of the information collected in the healthcare sites is communicated outwards to or through the other actors in the healthcare industry, namely the payers, claims switches, data bureaus, etc. Because electronic medical claims data is widely used, it is abundantly available by contrast to EMR data. Claims data is, however, an abbreviated form of the patient's care data because settling a claim does not require the full details of the patient's care. Nevertheless, even with this limitation, it can address the needs of most data applications. Claims data applications include patient population estimation and patient share, therapy progression analysis, drug dosing and titration, mode of therapy analysis, referral pattern analysis, drug use by indication, treatment adherence and patient persistency and compliance, source of business, physician segmentation and targeting, patient segmentation, direct-to-patient program analysis, epidemiology, diagnosed vs. treated patient population estimates, disease staging, co-morbidity analysis, burden of illness analysis, medical outcomes, time value of the patient, health and productivity analysis, reimbursement analysis, claims rejection and claims reversal analysis, price sensitivity analysis, co-pay analysis, and Medicare Part-D analysis.
Longitudinal patient data studies can be successfully completed when the data for subject patients is rather complete (all episodes of care) and spans a period over several months or years. Generally, there are two types of claims databases available. Closed panel databases having a finite number of patients with complete history of care, and open panel databases, having significantly larger number of patients, but with the patient's treatment history somewhat incomplete due to a rather random data collection process.
'Patient Data 101' provides a thorough coverage of the above concepts and applications of longitudinal patient data.